Doctors have a range of treatments they can recommend to men with premature ejaculation, including pharmaceutical treatments, therapy, and self-help.
There are also countless websites, adult stores and pharmacies selling a wide range of pills, sprays, gels and creams.
But what scientific evidence is there that the different treatment options make a difference?
In this article, I’ll be sharing some of the key research I’ve found. Hopefully, you’ll find it useful if you’re also interested in knowing what scientific research has proven to be effective.
Contents
- Is there a cure for premature ejaculation?
- Historical problems with the research
- The new definitions of lifelong and acquired premature ejaculation
- SSRI antidepressants research
- Dapoxetine research
- Tramadol
- Topical a
nesthetics - Behavioral techniques
- Kegel exercises
- Lifestyle factors
- PE and Erectile Dysfunction
- Conclusion
- Your views
1. Is there a cure for PE?
This is a crucial question, and it seems the answer is both yes and no.
It appears that there still isn’t a simple treatment that works the same for all men. It’s a complex problem with many possible causes, and sometimes a combination of causes.
So for now, it’s either a case of finding the most likely cause and corresponding treatment or some proactive trial and error until you find an option that helps.
Some men respond well to oral medication. Some have better results with topical anesthetics. And others may benefit from counseling or self-help techniques.
It also depends on what’s meant by the word ‘cure.’ If it’s to be able to last for as long as you want, then it’s perhaps harder to achieve for most men.
If you mean go from lasting just 1, 2 or 3 minutes to lasting 4, 5 or even longer, then yes it’s definitely possible.
2. Historical problems with research into PE
In 2008, doctors at the New Jersey Medical School published an interesting summary of peer-reviewed research into medical options.
They concluded that research into PE in the past had been ‘hampered’ by several factors, including:
- The complexity of the condition.
- Variation between men and different cultures.
- No standardized definitions.
- The subjectivity of PE, with questionnaires not being objective enough.
- A lack of properly controlled and assessed studies into different treatments.
They, among others, recommended that future research be more carefully designed and controlled.
However, that’s easier said than done. It’s understandably difficult to objectively assess PE and its treatment.
One of the main measurements is known as the Intravaginal Ejaculation Latency Time (IELT). This requires men to time themselves accurately and honestly using a stopwatch during sex.
Another key measurement is the level of satisfaction, which is prone to issues with subjectivity.
And in terms of research methodology, there can be various problems. For example, men being aware that they have the topical anesthetic rather than a placebo because they can clearly feel it working.
3. Research into the definitions of lifelong and acquired PE
In 2014, one of the above problems with research was dealt with by the International Society for Sexual Medicine (ISSM) AD Hoc committee for the definition of premature ejaculation.
They published the results of their extensive efforts to provide evidence-based definitions for both lifelong and acquired PE.
Their aim is to “enable researchers to design methodologically rigorous studies to improve our understanding of acquired PE.”
Here are their definitions:
On this basis, the committee agreed on a unified definition of both acquired and lifelong PE as a male sexual dysfunction characterized by (i) ejaculation that always or nearly always occurs prior to or within about 1 minute of vaginal penetration from the first sexual experience (lifelong PE) or a clinically significant and bothersome reduction in latency time, often to about 3 minutes or less (acquired PE); (ii) the inability to delay ejaculation on all or nearly all vaginal penetrations; and (iii) negative personal consequences, such as distress, bother, frustration, and/or the avoidance of sexual intimacy.
So it seems that the average lasting time during vaginal penetration is:
- Lifelong PE = 1 minute.
- Acquired PE = 3 minutes.
4. SSRI antidepressants research
Although never intended as a premature ejaculation treatment, doctors sometimes prescribe a type of antidepressant known as SSRIs (Selective serotonin release inhibitors).
These drugs, such as sertraline, paroxetine, and fluoxetine, have been shown in research to help men control their ejaculation, but come with the concern of side effects.
In the 2008 study I mentioned earlier, Doctors Sadeghi and Watson point out that SSRIs have historically shown the most success.
However, they also warn that there are side effects and worries about suicide rates among young men taking some of these drugs:
Selective serotonin release inhibitors have been the most promising agents to date. The on-demand “PRN” use of these agents is more convenient, but its efficacy is less well established. Chronic use of this class of medications has been associated with minor, but bothersome side effects. More recently, concern over the risk of an increased suicide rate in young men upon initiation of SSRIs has dampened enthusiasm.
Another issue with taking SSRIs is the fact that the original length of time during sex usually returns quite quickly once the medication is stopped, as researchers from Sao Paolo point out in 2011:
Cessation of treatment results in re-establishment of the previous set-point within 5 to 7 days in men with lifelong PE
5. Dapoxetine/priligy research

Since antidepressants need to be taken every day to be effective and carry the risk of adverse side effects, attempts have been made to create drugs that act in a similar way, but can be used on-demand.
Dapoxetine, also called Priligy, probably shows the most promise so far and can be taken just 1 to 3 hours before sex rather than every day.
In 2013, Australian researchers conducted a study involving 429 men who had an IELT of under 2 minutes, finding the following:
- IELT with dapoxetine was 5.2 minutes compared to 3.4 minutes with placebo.
- 56.5% of men considered their PE was better at the end of the study compared to 35.4% with placebo.
Subsequent research has also found dapoxetine to be effective. However, the results of a
The researchers report the following dropout rates:
Of all patients, 9.9% continued treatment to 2 years. The cumulative discontinuation rates at 1, 3, 6, 12, and 24 months were 26.4%, 61.6%, 79.1%, 87.3%, and 90.1%, respectively. Moreover, 79.1% of all patients discontinued treatment within 6 months. After 12 months, the discontinuation rate decreased sharply.
Park et. al.
6. Tramadol

In 2015, British researchers conducted a review of 8 randomized controlled trials into the use of Tramadol for PE.
Their findings were very interesting considering this is a drug which many men have discovered work for them, myself included.
Here are some of their findings:
- Tramadol was reported as significantly more effective than placebo for various patient-reported outcomes.
- One study showed tramadol to be more effective than Paroxetine. But another showed no significant difference.
- The dose of tramadol usually ranged from 25 mg to 89 mg.
- Tramadol is significantly more effective than sildenafil, lidocaine gel, or behavioral therapy.
- There were problems with the methodology and potential bias of many experiments. Nontheless, the results might not be affected significantly.
- Tramadol is associated with many adverse side effects, but they appear tolerable. However, the long-term safety and potential for addiction are still unclear.
- More research is needed to compare Tramadol with other treatments. The findings of research so far should be treated with caution considering the methodology of the research to date.
So it appears that studies have shown Tramadol to be effective. But at the same time, more research is needed before it can be deemed safe and more effective than other treatments.
As the study authors themselves concluded:
Tramadol appears more effective than placebo or behavioural therapy in the treatment of PE. However, these findings should be interpreted with caution given the observed levels of between-study heterogeneity and the methodological quality of the available evidence.
7. Topical anesthetics / desensitizing sprays and creams

Topical anesthetics, such as delay sprays and creams, are one of the most commonly available PE treatments.
They are widely sold on the internet, in sex shops, pharmacies and even in supermarkets.
In 2016, researchers at the University of Sheffield published
Similarly to the review of Tramadol research, they found issues with several of the studies’ methodology. Nonetheless, the results of the 9 studies they looked at are interesting.
This is an important treatment to study, as topical anesthetics are also one of the main treatment options doctors recommend. As the study authors state:
the European Association of Urology guidelines for the management of PE recommend on-demand topical lidocaine–prilocaine cream
Some of their key findings were:
- EMLA cream had a significantly better IELT (duration during sex) than placebo.
- TEMPE spray (now known as Fortacin) had a better IELT than placebo.
- At the end of one study, there was increased sexual satisfaction from using a lidocaine gel.
- One study showed better feelings of sexual satisfaction after 2 months when using EMLA.
- 1 study showed no difference in sexual satisfaction between TEMPE and placebo after 4 weeks. But 2 other studies showed that after 2 months TEMPE was more effective than placebo for sexual satisfaction and ejaculation control.
- One study showed lidocaine gel was better than sildenafil and paroxetine.
- Tramadol was significantly more effective than lidocaine gel in terms of IELT and sexual satisfaction.
So it seems then that the topical anesthetics which have been studied are significantly more effective than a placebo, and potentially better than some oral treatments, with the exception of tramadol.
Interestingly, in terms of side effects there was a considerable difference:
- Anesthetics: reduced sensitivity, numbness and irritation/burning for men and their partner. In some cases, erectile dysfunction and erection loss.
- Tramadol, sildenafil, and paroxetine: sleep problems, dry mouth, nausea, dizziness, fatigue, vomiting, sweating, and headache.
Despite these side effects, they also report than most men appeared to tolerate the side effects, presumably accepting the trade-off for better sexual satisfaction.
The study authors also comment on the potential pros and cons of topical anesthetics, saying:
Systemic adverse events were more prevalent with oral treatments, which may make topical anaesthetics more acceptable. Likewise, the rapid action of topical anaesthetics compared with planning to take oral medication in advance might also be more acceptable. Conversely, the inconvenience of washing and transfer of the agent to the partner might be limiting factors to acceptability
And finally, they conclude that:
Topical anaesthetics appear more effective than placebo, paroxetine and sildenafil at increasing IELT in men with PE. However, these findings should be interpreted with caution given the limited methodological quality of the available evidence.
8. Behavioral techniques
Until now I’ve looked at different pharmaceutical approaches to treatment. And research has, perhaps unsurprisingly, focused heavily on such medical treatment.
However, it’s important to also consider behavioral options. This is something online advice tends to focus on, since it offers a self-help option to men who don’t feel comfortable speaking to their doctor about PE, or who prefer not to take medication.
As well as self-help, this pathway might also include psychotherapy (psychosexual or relationship counseling) for men or couples.
In their 2011 research paper, researchers from St James University Hospital at Leeds university discuss the difference in approaches, saying:
This fundamental controversy about whether PE is behavioural or biomedical has been reflected in the two differing approaches to therapy (i.e. behavioural or psychotherapy versus pharmacological therapy).
They looked at the evidence for classic behavioral techniques, such as the start and stop method and the squeeze technique.
They mention a 1986 research study which found short-term success with these techniques in 45%-65% of men, but a lack of long-term evidence, saying only 25% of men had lasting improvement.
And in 2015, British researchers conducted a review of behavioral techniques. They looked at 10 randomized controlled trials involving 521 participants.
Here are some key findings:
- 2 out of 4 studies reported behavioral therapies improved IELT compared to being on a waiting list for treatment.
- 1 study showed an increase of nearly 7 minutes from functional-sexological treatment or behavioral compared to placebo (1 group receiving education on sensuality, body movement, the speed of sex, muscular tension and breathing. The other the start-stop and squeeze technique.) The positive effect continued 3 months later. The level of sexual satisfaction and perceived control was also significantly improved in all 3 groups.
- 1 study found using a hand-held masturbation device improved IELT by 1.6 minutes, and 1.7 minutes at 6-month follow-up.
- 1 study compared 3 options to no treatment: self-help book alone, book with
therapist phone contact, couples therapy. They found all 3 options improved IELT by 7-9 minutes. And after 3-6 months, the improvement was still significant. - I study found no significant improvement from
a web-based sex therapy compared to no treatment. One study found significant improvements in IELT, men’s perception of duration during sex, and the couple’s feeling of sexual satisfaction after doing either the start and stop technique or sensual focusing.
In addition, they also investigated research studies that had combined behavioral therapy with drug treatment, finding the following:
- Behavioral therapy combined with chlorpromazine gave a 1-minute improvement compared to chlorpromazine alone after 6 weeks.
- Behavioral therapy combined with paroxetine was slightly better than paroxetine alone.
- Behavioral therapy combined with citalopram was 0.5 mins better than just citalopram.
- Sildenafil or Paroxetine was better than the squeeze technique. But there was no difference between the squeeze technique and sertraline or clomipramine.
- One study found perceived ejaculation control was better with paroxetine than behavioral techniques. But patient and partner satisfaction was better with behavioral techniques.
- There was no difference in one study in sexual satisfaction between the start and stop technique of fluoxetine.
- Another study found sildenafil or paroxetine gave better satisfaction that the squeeze technique. But there was no difference between the technique and clomipramine or sertraline.
And perhaps importantly for men who worry about medical treatment, there were no adverse effects recorded for any of the behavioral techniques in all 10 studies looked at.
Despite saying that most of the studies had methodological flaws – as seems to be the case with much PE research – they do conclude that there is evidence that behavioral technique can help:
There is limited evidence that physical behavioral techniques for PE improve IELT and other outcomes over waitlist control. There is also some evidence that BTs combined with drug treatments improve IELT and other outcomes compared with drug treatments alone.
9. Kegel exercises
For me,
However, since the research I’ve looked at focuses more on techniques like the start and stop method, the squeeze technique, sensate focusing etc, I’ll look at kegels separately.
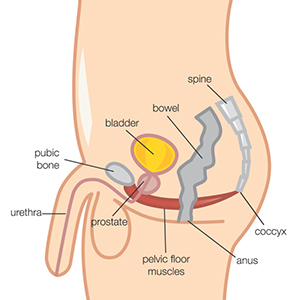
Kegel exercises feature heavily in self-help articles online. Most articles I’ve read tell men to work on their pelvic floor muscles.
In 2014, Italian researchers studied the effect of pelvic floor rehabilitation for men with lifelong PE, with promising results.
Although the men received physio-kinesiotherapy and electro-stimulation of the perineal floor to work on their pelvic floor muscles, they were also taught to identify the correct muscles and then exercise them by doing kegels.
They found that:
- 33 out of 40 men were able to gain ejaculation control, and improve their IELT.
- At the outset, the average duration during sex was 31.7 seconds. After 6 weeks it rose to 124.6 seconds. And after 12 weeks 146.2 seconds.
- The men who returned for the 6 month followup reported continued positive effects.
Importantly, they also provided an insight into the on-going debate about
In addition, we demonstrated that active perineal muscle control inhibits the ejaculation reflex through intentional relaxation of the bulbocavernous and ischiocavernous muscles, which are active during arousal and should be intentionally relaxed during this phase of sexual intercourse. This is an easily learned technique that can be mastered by using pelvic floor biofeedback.
Yoga and the pelvic floor
Indian researchers in 2013 conducted a small experiment with 12 men to see if Yoga or naturopathic procedures would help with PE.
On closer inspection, I discovered that one of the major Yoga techniques was similar to kegels. They found no significant improvement to PE after 21 days. However, they did note that there was some improvement, and so perhaps it would help over a longer time period.
In 2016, researchers in San Diego conducted a review of data on the role of pelvic floor muscles in sexual dysfunction.
They looked at the current scientific understanding of the role the muscles play as well as past research studies, saying:
Pelvic floor therapy has been shown to improve control over ejaculatory delay and allow significant increases in intravaginal ejaculatory latency times in men with pelvic floor muscle dysfunction
And interestingly, they also note how there continues to be some mystery surrounding the exact way to work on the pelvic floor muscles, saying:
The application of pelvic floor therapy to the treatment of premature ejaculation is safe and effective, although studies have not yet specifically identified how to appropriately implement muscular strategies. Whether emphasis should be on strength, control, or relaxation is not yet well understood; therefore, current treatment should be tailored to individual
findings
10. Lifestyle factors
Exercise and PE
In 2016, researchers in Finland found a correlation between physical exercise and PE. They recommend that if future research repeats their findings, then physical exercise could be added to a treatment regime.
Age, smoking, BMI
In 2013, Chinese researchers published the results of a large piece of research involving 3016 men.
25.80% of the participants said they had PE. On average they were older, more likely to smoke, with a higher Body Mass Index (BMI) and more co-morbid health problems. They also found more men with PE were already receiving counseling from a doctor.
11. The interplay between PE and Erectile Dysfunction
Some researchers and doctors study the link between PE and Erectile Dysfunction (ED).
However, as Italian researchers point out in 2016 in their large study, the link still isn’t clear:
The specific determinants and underlying factors linking erectile dysfunction (ED) and premature ejaculation (PE) have yet to be clearly identified.
In their study, they looked at 18 previous pieces of research, involving a total of 57,229 patients, of whom 21.22% had PE. And they found that PE was associated with a significantly increased risk of ED.
Furthermore, they found the risk of ED in patients with PE in certain categories, such as:
- Older men.
- With a lower level of education.
- Reported less frequent stable relationships.
- More anxiety and depressive symptoms.
- Higher risk in men with acquired PE.
- Less physical comorbid conditions such as diabetes and hypertension.
Treat ED before PE
In cases where men do suffer from both PE and ED, the American Urological Associated guidelines suggest treating the ED first, offering this explanation as to why:
Many patients with ED develop secondary PE, perhaps due to either the need for intense stimulation to attain and maintain an erection or due to the anxiety associated with difficulty in attaining and maintaining an erection. Premature ejaculation may improve in patients when concomitant ED is effectively treated.
Conclusion
It appears that there is scientific evidence that most PE treatments have the potential to help some men. But none have been proven to help every man with PE who tries the treatment.
How well they work varies from one type of treatment to the next, one man to the next, and even one research study to the next.
Careful reviews of the many smaller research projects have shown that there are often fundamental flaws in the research methodology. This doesn’t make it easy for members of the public who are interested in the research to work out how well a treatment truly works.
Despite the criticisms that some authors have though, there does seem to be evidence that a range of oral drugs, topical anesthetics, and behavioral techniques work. And some men may further benefit from combining medical and behavioral treatments.
So as I suggested in the beginning, for now at least, men will have to make informed choices about which treatment to try. If they feel able to speak to their doctor, they will gain access to a wider range of medical treatments.
And with their doctor or therapist’s support, or alone through self-help, men can try a range of topical anesthetics and behavioral techniques.
You might also like
If you made it to the end of this huge article, I’m impressed! And if you still have the energy to read more, you might like to check out my main overview of premature ejaculation self-help treatments.